
Postnatal exposure to sedatives, hypnotics or narcotics. Drugs - Prenatal exposure with transplacental transfer to the neonate of various drugs (narcotics, beta-blockers).Temperature Regulation - Hypothermia or hyperthermia.Gastrointestinal - NEC or gastroesophageal reflux.Metabolic - Hypocalcemia, hypoglycemia, hyponatremia or acidosis.
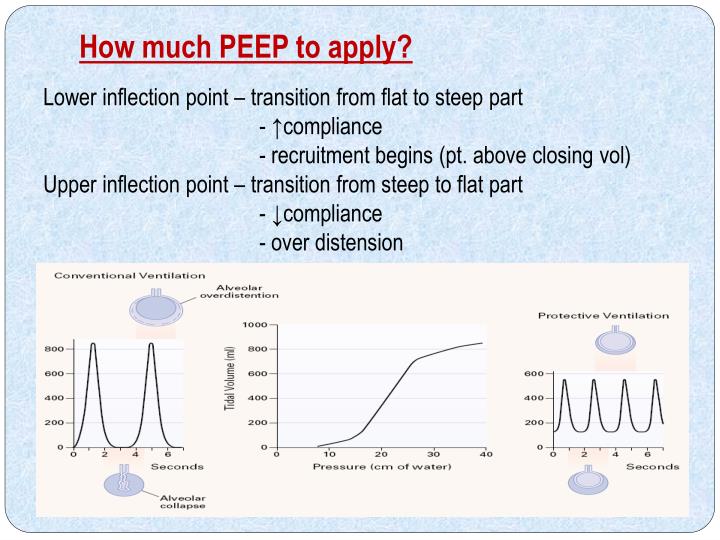
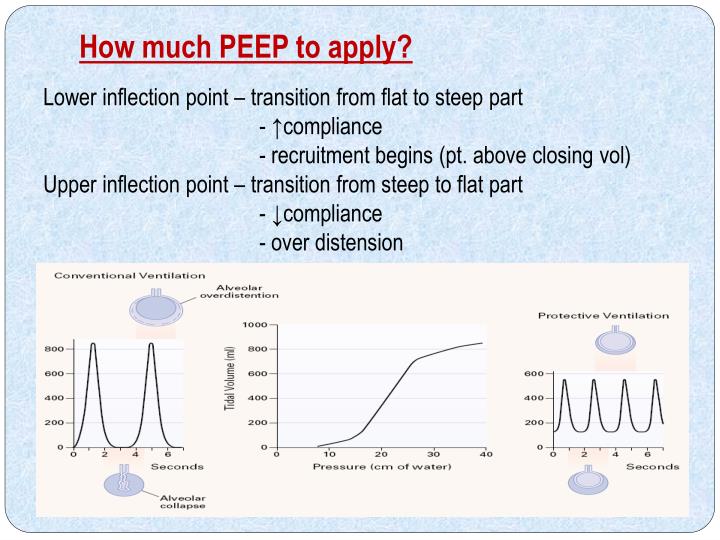 Pulmonary - Impairment of oxygenation and ventilation from lung disease (surfactant deficiency disease, pneumonia, transient tachypnea of the newborn, meconium aspiration, etc.). Cardiovascular - Impairment of oxygenation from congestive heart failure and pulmonary edema (PDA, coarctation, etc.), or from shunting (cyanotic heart disease). Neurological - Intraventricular hemorrhage, intracranial hemorrhage, neonatal seizures, perinatal asphyxia, or other pathology which could lead to increased intracranial pressure. Infection - Sepsis, especially in the first day of life, and nosocomial infections and/or NEC in the first weeks of life. The most common cause of apnea in the NICU is apnea of prematurity, but first ALWAYS investigate and rule out the following disorders: SequelaeĪpnea in premature infants can result in a failure of the mechanisms that protect cerebral blood flow, resulting in ischemia and eventually leukomalacia.ĭuring apneic episodes, in an attempt to protect cerebral blood flowcardiac output is diverted away from the mesenteric arteries resulting in intestinal ischemia and possibly necrotizing enterocolitis (NEC). Apnea at UIHC is defined as cessation of breathing for 20 seconds with the above symptoms. Measurement of ventilator pressures, flow and volume before/during/after the PV curve.Peer Review Status: Internally Peer Reviewed DefinitionĪpnea is a "pause in breathing of longer than 10 to 15 seconds, often associated with bradycardia, cyanosis, or both." (Martin et al). Reconstruction of EIT derived PV curve will determine, first: if there is a left and/or right lung airway closer phenomenon, and second: the value of each lung AOP. PV curve on the ventilator will be analysed to determine if there is an airway closer phenomenon. A classical low flow PV curve from without PEEP will be done, the acquisition of EIT data during PV curve will be analysed secondary with a dedicated software. PEEP will be titrated with PEEP-EIT method. Patients with moderate to severe ARDS equipped with EIT will be included. It is therefore important to describe specifically Covid 19 patients with ARDS.
Pulmonary - Impairment of oxygenation and ventilation from lung disease (surfactant deficiency disease, pneumonia, transient tachypnea of the newborn, meconium aspiration, etc.). Cardiovascular - Impairment of oxygenation from congestive heart failure and pulmonary edema (PDA, coarctation, etc.), or from shunting (cyanotic heart disease). Neurological - Intraventricular hemorrhage, intracranial hemorrhage, neonatal seizures, perinatal asphyxia, or other pathology which could lead to increased intracranial pressure. Infection - Sepsis, especially in the first day of life, and nosocomial infections and/or NEC in the first weeks of life. The most common cause of apnea in the NICU is apnea of prematurity, but first ALWAYS investigate and rule out the following disorders: SequelaeĪpnea in premature infants can result in a failure of the mechanisms that protect cerebral blood flow, resulting in ischemia and eventually leukomalacia.ĭuring apneic episodes, in an attempt to protect cerebral blood flowcardiac output is diverted away from the mesenteric arteries resulting in intestinal ischemia and possibly necrotizing enterocolitis (NEC). Apnea at UIHC is defined as cessation of breathing for 20 seconds with the above symptoms. Measurement of ventilator pressures, flow and volume before/during/after the PV curve.Peer Review Status: Internally Peer Reviewed DefinitionĪpnea is a "pause in breathing of longer than 10 to 15 seconds, often associated with bradycardia, cyanosis, or both." (Martin et al). Reconstruction of EIT derived PV curve will determine, first: if there is a left and/or right lung airway closer phenomenon, and second: the value of each lung AOP. PV curve on the ventilator will be analysed to determine if there is an airway closer phenomenon. A classical low flow PV curve from without PEEP will be done, the acquisition of EIT data during PV curve will be analysed secondary with a dedicated software. PEEP will be titrated with PEEP-EIT method. Patients with moderate to severe ARDS equipped with EIT will be included. It is therefore important to describe specifically Covid 19 patients with ARDS. 
Phenotypes are discussed with differences in terms of respiratory mechanics. Recent Covid 19 pneumoniae is responsible for numerous acute respiratory distress with severe hypoxemia. The investigor wants to compare global AOP on ventilator PV curve with left and right lung EIT derived AOP measurements. EIT is an interesting monitoring tool that could allow EIT derived PV curve construction with measurement of regional AOP2, right vs left lung. However, this will measure a global AOP whereas ventilation is heterogeneous between the two lungs in ARDS. The detection of airway closure and the measurement of AOP need a pressure volume curve at low flow and no positive end expiratory pressure (PEEP). Recent research demonstrates that airway closure is a matter of concern as it participates to the heterogeneity of tidal ventilation distribution and it can amplify Ventilator Induced Lung Injury (VILI). This phenomenon of airway closure has been underestimated and misinterpreted. In one third of Acute Respiratory Distress Syndrome (ARDS), tidal inflation starts when an airway opening pressure (AOP) is overcome 1. Why Should I Register and Submit Results?.





 0 kommentar(er)
0 kommentar(er)
